To define ‘what is patient safety?’, it is critical to distinguish the difference between ‘patient safety’ and ‘Laboratory safety’. ‘Patient safety’ focuses on preventing errors associated with the provision of laboratory services and striving to improve care for the patient. ‘Laboratory safety’ focuses on keeping laboratory professionals safe as they perform their assigned duties. Both forms of safety are extremely important, however they are not the same nor are the terms interchangeable.
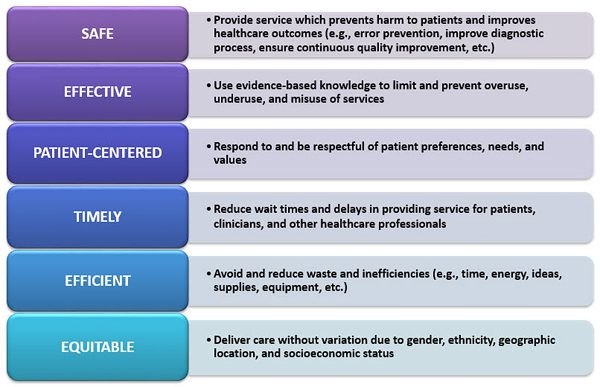
Patient Safety is focused on ‘Do No Harm’ which includes avoiding harm to patients from the care that is intended to help them. “Medical Laboratory Professionals are stewards of patient safety and must promote a culture of safety and quality defined by the Institute of Medicine (IOM, now the National Academy of Medicine) as safe, effective, patient-centered, timely, efficient, and equitable practice.”1
IOM’s Six Quality Aims For Healthcare 2
How do these quality aims directly relate to the practice of Laboratory Medicine?
With each of the six quality aims, there exists tremendous opportunity for medical laboratory professionals to not just work towards ‘error prevention’ but to focus all phases of laboratory services on improving patient outcomes. Studies have been published that demonstrate the importance of strategically assessing and improving all phases of the ‘total testing process (TTP)’ (e.g. preanalytical, analytical, postanalytical phases). Laboratory professionals and technological advancements have improved the analytical phase of the TTP so that it now harbors the least amount of error. It is now important for laboratory professionals to focus efforts on the preanalytical and postanalytical phases of the TTP. In these phases, the current most vulnerable and error prone processes include: selecting the correct test to order (preanalytical); accurately interpreting test results (post analytical); reporting test results to the patient (postanalytical).3
With each required laboratory process included in the separate phases of the TTP, the process may be evaluated based on how it meets each of the six aims. Through in-depth evaluation, weaknesses in process may be identified and allow for development of new or revision of current process that will improve outcome, quality and patient safety. Many of the processes in the preanalytical and postanalytical phases will require laboratory professionals and laboratory teams to step out from the boundaries known as ‘under direct laboratory control’. Actions should include requesting to form or volunteering to serve on interdisciplinary teams. Success will happen through direct partnerships which are focused on building trust and open, positive lines of communication with physicians, nurses, other healthcare professionals, patients and families. All healthcare leaders and professionals must feel compelled and empowered to uphold mutual accountability and speak up for safety.
How can I, as a laboratory professional, positively impact patient safety?
- Ensure that patient safety is recognized as a core value in the mission of your laboratory and is a top priority for you as a practicing healthcare professional
- Assist in and support building a laboratory culture in which all leaders and professionals understand the basic principles of patient safety and assure that patient safety continuing education is available for all staff
- Commit to and support the principles of a ‘just culture’ within the laboratory. A ‘just culture’ “focuses on identifying and addressing system issues that lead individuals to engage in unsafe behaviors, while maintaining individual accountability by establishing zero tolerance for reckless behavior.” (AHRQ PSNet 2016)
- Commit to and support behavior expectations for the workforce that contribute to improving patient safety (e.g. transparency, effective teamwork, open communication, just culture, respect, and direct and timely feedback)
- Incorporate the IOM identified patient safety competencies4 into your daily practice:
- Provide patient-centered care – recognize the patient is the focus of your practice
- Employ evidence-based laboratory practice to facilitate and support change
- Apply quality improvement principles to processes to reduce opportunities for error and improve service delivery
- Use informatics as an essential component of your practice and to enhance communication to provide safe healthcare delivery
- Work on interprofessional healthcare teams to provide laboratory expertise in developing innovative and improved healthcare services
References
- ‘Patient Safety and Clinical Laboratory Science’ ASCLS Position Paper
- Committee on Quality of Health Care in America. Institute of Medicine. Kohn L, Corrigan J, Donaldson M., eds. To err is human: building a safer health system. Washington DC: National Academy Press; 2000.
- Plebani,M. Diagnostic errors in laboratory medicine-causes and strategies; The Journal of the International Federation of Clinical Chemistry and Laboratory Medicine; eJIFCC 2015; Vol 26 No1; pp007-014
- Committee on the Health Professions Education Summit, National Academies Press. Greiner AC, Knebel E, eds. Health Professions Education: A Bridge to Quality. Washington DC: National Academies Press; 2003.
Additional resource articles on ‘What is Patient Safety’
- Otto CN. Patient safety and the medical laboratory, an introduction. Clin Lab Sci, 2011; 24(2): 105-107.
- Otto CN. Patient safety and the medical laboratory using the IOM aims. Clin Lab Sci, 2011; 24(2): 108-113.
- Morris S. Just culture–changing the environment of healthcare delivery. Clin Lab Sci, 2011; 24(2): 120-124.
- Golemboski K. Improving patient safety: lessons from other disciplines. Clin Lab Sci 2011; 24(2): 114-119.
- Morris S, Otto CN, Golemboski K. Improving patient safety and healthcare quality in the 21st century-competencies required of future medical laboratory science practitioners. Clin Lab Sci 2013; 26(4): 200-204.