Did You Know?
- A diagnostic error is “the failure to (a) establish an accurate and timely explanation of patient’s health problem(s) or (b) communicate that explanation to the patient.” [1]
- It is likely that most of us, as health care consumers, “will experience at least one diagnostic error in our lifetime, sometimes with devastating consequences” [2]
- It is estimated that diagnostic errors affect 12 million Americans each year in outpatient settings and may seriously harm one-half or 6 million of these patients [3]
- Conservative estimates suggest that 40,000-80,000 Americans die each year from diagnostic failures in U.S. hospitals alone [4] [On average: “Every nine minutes, someone in a U.S. hospital dies due to a diagnostic failure”]
- A Johns Hopkins study released in May 2016, calculates that “more than 250,000 deaths per year are due to medical error in the U.S.” [5]
Patient Safety in Laboratory Medicine Matters
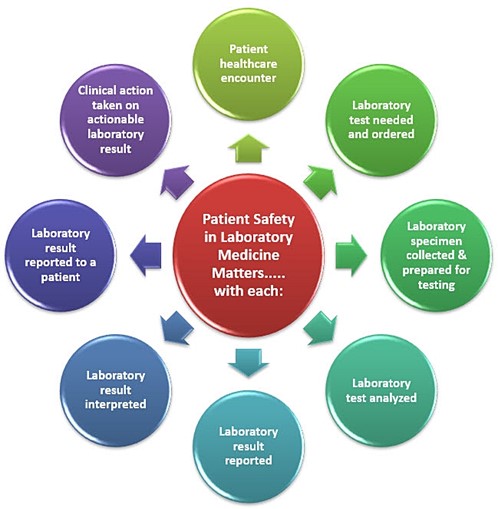
Figure 1: Total Testing Process [6]
All healthcare should be safe, effective, patient-centered, timely, efficient, and equitable. [7]
As one of the leading diagnostic service lines in healthcare, patient safety in laboratory medicine matters.
In all phases of the laboratory total testing process, medical laboratory professionals have the ability and responsibility to improve patient safety and health outcome.
Patient Safety-Centered Laboratory Services
Patient safety-centered laboratory services assure care that avoids harm to patients, enhances safe care outcomes through error prevention, allows continuous process improvement, and assures appropriate levels of care are provided to each patient served. The aim of laboratory medicine and its practitioners as stewards of patient safety is to provide services focused on providing safe care and improving patient health outcomes throughout the total testing process which includes all phases of laboratory testing from the time a laboratory test should be ordered, to when the laboratory test result is reported to the clinician, interpreted, and the result is reported to the patient. [6]
Drivers of Change
The primary drivers of the patient safety movement include reports from the National Academy of Medicine as well as requirements identified by national accrediting and regulatory agencies (e.g., Center for Medicare & Medicaid Services (CMS) CLIA [8], College of American Pathologists (CAP) [9], COLA [10], The Joint Commission [11]). The focus of this change is to monitor performance to improve patient safety and health outcome.
National Academies of Sciences, Engineering and Medicine
In 1999, The National Academy of Medicine (then known as The Institute of Medicine) published a landmark report titled To Err is Human. [12] This report described an epidemic of preventable medical errors in healthcare and identified gaps in healthcare delivery as the source of the errors. “These gaps were created by faulty systems, processes, and conditions which either lead to or failed to prevent mistakes by healthcare workers.” [12] An additional report, Crossing the Quality Chasm [7], advised healthcare systems to implement safe practices within their delivery models and recommended six quality aims for healthcare that promote a culture of safety and quality. [7]
The six quality aims are:
Figure 2: Six Quality Aims for Healthcare
In 2015, more than a decade after To Err is Human [12] was published, Improving Diagnosis in Healthcare [1], was published by the National Academy of Medicine. This report was directed to all healthcare providers and services involved in the diagnostic process. Specific to laboratory medicine, this report:
- “acknowledges the critical role of pathology and laboratory professionals in the diagnostic process”
- “documents that patient safety, improvement in the diagnostic process, and reducing diagnostic errors are the responsibility of all healthcare professionals, including laboratory professionals”