What is a Patient Safety Indicator?
Patient safety quality indicators are healthcare’s equivalent to key performance indicators (KPI) used in the business world. A KPI is something that can be measured and is used to demonstrate to everyone that the company is achieving its key business objectives. [13]
In healthcare, one of the key “business” objectives is to keep patients safe from adverse events. We call healthcare KPIs “patient safety quality indicators” (PSQI) or “patient safety indicators” (PSI) or just quality indicators. According to the Agency for Healthcare Research and Quality (AHRQ), these indicators are measurements that screen for adverse events that patients might experience because of their interaction with the healthcare system. As AHRQ states “These events are likely amenable to prevention of adverse events by changes at the system or provider level.” [14]
PSIs should be evidence-based and focus on what matters most, considering personnel and other resources. [14] There is a common saying in the world of quality improvement – “What gets measured gets done.” Another way to think about this is, in order to improve a process or an outcome, one needs to measure that process or its outcome. In healthcare and in laboratories, it is essential to measure any process, procedure, or practice that may adversely impact patient outcomes or has the potential to improve healthcare outcomes using well-planned, inclusive patient safety indicators.
What is the Importance of Selecting an Appropriate Patient Safety Indicator?
Selection of appropriate PSIs are a means of evaluating and improving the effectiveness of a process or procedure. Identification of areas of improvement have the ability to not only decrease errors and improve processes but also can lead to performance comparisons with other laboratories. PSIs that are designed to allow peer-to-peer comparison (benchmarking) lead to evidence-based improvement, sharing of best-practices, and achievement of desired state-of-the-art services.
The individual PSI selected must specifically address dimensions of clinical performance and areas for improvement. Data needs to be collected over time to identify, correct, and continuously monitor areas that may adversely impact patient safety, diagnosis, and health outcome. Implementation of continuous corrective interventions using standardized processes will improve performance as well as patient safety.
When possible, the use of nationally defined or literature based PSIs supports needed harmonization to collect data that are comparable and allow direct interlaboratory comparison. These harmonization efforts include a common definition of the data elements of a PSI (e.g., numerator, denominator, rate expression calculation). [15] As an example, if one laboratory expresses data as # events per patient days, and another tracks the same event as a percentage of daily laboratory tests, those two cannot be directly compared and therefore do not contribute to comparative evaluation. The ability to compare performance to other laboratories allows:
- quantification of performance quality
- establishment of improvement priorities based on best-practice standards
- determination of improvements that are meaningful to patient safety and health outcomes
- effectiveness assessment of interventions
- establishment of standardized reporting systems
Questions to consider in assessing the appropriateness of a patient safety indicator include:
- Does the indicator evaluate and identify areas that pose the greatest risk of harm to patients or have potential to improve service outcomes?
- Does the indicator monitor and evaluate performance of a critical but specific phase of testing (pre-analytical, analytical, post-analytical)?
- Do additional indicators need to be added to assure complete assessment?
- Does the indicator assess one of the six quality aims of healthcare? (e.g., safe, effective, patient-centered, timely, efficient, equitable)
- Is the performance indicator aligned with the organization’s or laboratory’s patient safety initiatives?
Each step of the laboratory Total Testing Process that relates to the patient safety indicator selected needs to be carefully examined from a systems perspective for potential errors (defects in the process). This can be completed by performing an initial (trial) assessment of the defined patient safety indicator. The assessment should include determining where in the process or procedure an improvement is needed or needs to be sustained. Additional questions may then be asked to assess if the defined indicator will lead to achieving the initial desired outcome. Examples are:
- Have all departments that have responsibilities in the process (e.g., laboratory, nursing, information technology, outreach clients, physicians) been identified?
- Do they need to be included in the team responsible for achieving the indicator goal?
- Have any critical total testing process steps that can impact the indicator outcome been overlooked?
- Will the data required be consistently available as defined by the indicator?
- Does the data gathered allow identification of systems or processes that need to be improved to achieve the desired outcome?
- Will the data analysis required provide meaningful statistics and allow identification of possible interventions to achieve the improvement desired?
- Are the target and threshold limits set appropriate to achieve the desired outcome?
- Are revisions to the PSI definition required?
- Are any notifications necessary before the quality indicator process begins?
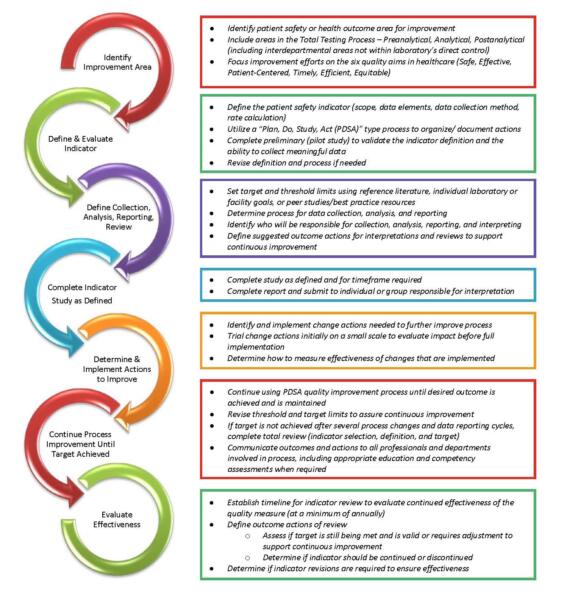
Steps in Selecting, Defining, and Evaluating a Patient Safety Indicator (PSI)
Select a specific patient safety or health outcome improvement area to be measured
- Patient safety and outcome improvement emphasis includes:
- Assessing the total testing process (pre-analytical, analytical, post-analytical)
- Assessing diagnostic and service processes based on the six quality aims for healthcare (safe, effective, patient-centered, timely, efficient, equitable)
- Some common sources to consider for identifying areas to improve patient safety include patient safety alerts (national and institutional); review of the published clinical laboratory science literature; the facility’s patient safety officer and risk management department; complaints received from providers, nurses, patients; incident reports; and reports of service failures from laboratory personnel.
- Areas to be measured should not just include areas within the direct control of the laboratory. The areas should also include processes for which control and responsibility are shared with other departments (e.g., point-of-care testing, specimen collection by non-laboratory professionals) within the organization or with external customers (e.g., patients, outreach clients and ordering clinicians).
- Refer to APPENDIX 1: Total Testing Process – Examples of Patient Safety Indicators
Define the PSI and requirements to measure performance
Using standardized PSI development forms assist with defining the indicator and allow for standardization when developing multiple indicators. (Refer to Section 3: Tools & Resources-Customizable Templates)
Suggested components in defining the indicator: [18]
- Indicator name and the purpose of the indicator (what improvement is desired)
- Scope of the indicator
- Phase of the total testing process the indicator is assessing (pre-analytic, analytic, post-analytic)
- Scope of testing included in indicator (e.g., hematology, chemistry, point-of-care, specimen collection)
- Department(s) that have responsibilities in the process (e.g., laboratory, nursing, information technology, outreach clients, physicians)
- Data elements to be collected or excluded for consistent data collection and rate calculation (e.g., unique identifier, sex, age, date, time, patient population, test result or specific limit criteria for test results to be reported)
- Method of expressing the PSI and its formula for calculation (e.g., occurrence frequency per day or per admission or per month or per tests reported) including the numerator and denominator definition
- Numerator = the number of times the parameter of the measure occurs (e.g., number of hemolyzed specimens, number of patients, number of result errors, number of transfusion reactions, number of incorrect tests ordered)
- Denominator = the total number (whole/entire) of the population being evaluated to obtain the statistical value desired for the rate expression (e.g., per total tests, day, admission, accession)
- Rate Expression Example: Percent of hemolyzed blood specimens received in the laboratory per total specimens received
- Numerator: number of hemolyzed specimens received during the study timeframe
- Denominator: total number of specimens received during the study timeframe
- Data collection method (e.g., data sampling frequency, data source(s), method to record data, timeframe for collection)
- Utilization of a commonly used quality improvement process, Plan-Study-Do-Act (PDSA) cycle [16] or other similar quality process, is helpful in organizing and documenting actions required with making changes to the PSI and testing impact of improvement changes. (Refer to Section 3 – Tools for PDSA cycle resources)
- Complete a preliminary data collection (pilot study) using the defined indicator is recommended to assess the definition of the PSI and to ensure required data can be obtained. If needed, adjustments to the definition may be made to provide meaningful data for the criteria being measured.
Define the PSI analysis and interpretation responsibilities
- Determine the target for the PSI (desired level of performance; value or outcome to be achieved) [18]
- Target may be from an external source (document the resource or reference utilized)
- Target may be established internally (e.g., organization or department goals, customer expectations)
- Determine the indicator threshold (predefined decision point set to trigger further evaluation and action when it is exceeded) [17]
- Revise threshold when needed to ensure continuous improvement
- Define who is responsible for collecting data, analyzing data, selecting data display format, and preparing the report; define timeframes that assignments must be completed by
- Define who is responsible for report interpretation, determination of improvement actions to be taken, change impact assessment, specific follow up required, and completion dates
- Continue utilizing the PDSA cycle quality improvement process until desired outcome is achieved and maintained
- Emphasize the importance of developing and implementing additional change actions with each data cycle to continuously improve the process
- Provide communication of outcomes and actions to all professionals and departments involved in the quality process, including appropriate education and competency assessments when required
Evaluate the PSI effectiveness and sustain improvement
- Establish a timeline for PSI review to evaluate the effectiveness of the PSI (at a minimum of annually) [18]
- During the review, determine if
- Target is still appropriate or needs to be adjusted to demonstrate continuous improvement
- Target is being continuously met and if the indicator should be continued, discontinued, or discontinued but requires a future scheduled study to validate sustainment
- Target is not attained and progress to achievement is not evident (requires complete evaluation and revision of PSI if indicated)
- Determine if indicator changes are required to ensure continued effectiveness
Figure 3: Patient Safety Indicator – Selection, Definition, and Evaluation Flow
- Refer to APPENDIX 2: Case Study – Patient Safety Indicator Example
- Tools to assist in selecting and defining patient safety indicators are found in Section 3 – Tools and Resources