Floyd Josephat, EdD, MT(ASCP)
The clinical education practicum serves as an intricate connector in our journey from the classroom curriculum to real work responsibilities. It has become a key component in both hospital and university-based clinical laboratory science programs. This key component in the curriculum of our profession is sometimes overlooked. However, it is becoming more visible as our profession continues to grow and people begin to recognize the value in what we do.
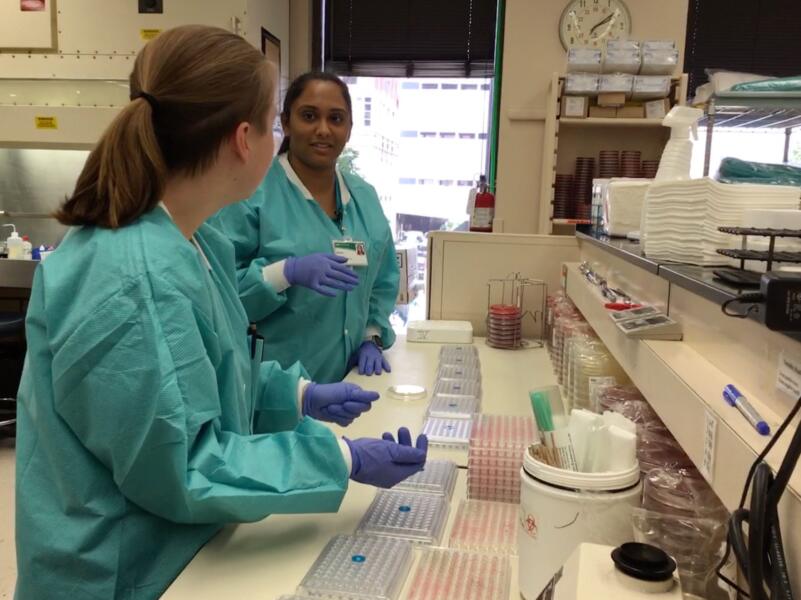 |
| Clinical laboratory science preceptors work to make sure CLS students get the most current laboratory training experiences that are needed to function in today’s scientific work environment. |
Connecting what we are learning in the classroom can be challenging because of the complexity of some subjects, but it is still an important way of integrating classroom learning objectives into real work settings. A clinical practicum can provide the opportunity for students to observe clinicians in practice, apply their classroom knowledge, and develop ethical and moral decision-making skills in providing patient care as they begin to assume their professional identity (Romig, Tucker, Hewitt, and Maillet, 2016).
Clinical Training Overview
Clinical training has also been defined as “the practice of assisting a student to acquire the required knowledge, skills, and attitudes in practice settings, to meet the standards defined by a university degree structure or professional accrediting/licensing board” (Rose & Best, 2005, quoted in Romig et al., 2016, p. 244). While classroom education and controlled laboratory and simulation experiences provide essential background knowledge and basic skills, clinical training or practicum deliver the most value to students and to the hospitals and other clinical settings that will employ them after graduation (Sepples, Goran, & Zimmer-Rankin, 2013).
Clinical training involves placement of a student at a clinical site under the supervision of a practicing clinician serving as a preceptor. This model provides the student with real-life experiences that work toward developing students into confident and competent practitioners. Some of the goals of clinical training are to help the student:
- Apply theory and learning to clinical practice,
- Orient to professional behaviors and attitudes in the clinical workplace,
- Hone and refine, through observation and repetition, the skills required for clinical practice,
- Develop communication and collaboration skills to function within an interprofessional healthcare team, and
- Develop skills in critical thinking, problem-solving, and time management in the fast-paced clinical setting (Romig et al., 2016).
The Role of Site Preceptors
The training of future clinical laboratory science (CLS) students depends heavily upon the availability and expertise of site preceptors. Some of these preceptors are highly trained individuals in specialty areas such as hematology, immunohematology, microbiology, chemistry, coagulation, immunology, and molecular diagnostics. They are also classified as non-faculty but are practicing clinical laboratory scientists at the clinical site.
Their purpose is to provide a one-on-one clinical experience in each of the sub-specialty areas with the student. Students develop clinical skills and competencies that are gained from practical experience working with the preceptors and other members of the healthcare team. These are valuable training experiences that are given to students freely and on a continuous basis. Clinical laboratory science preceptors work tirelessly to make sure that CLS students get the most current laboratory training experiences that are needed to function in today’s scientific work environment.
Some of their responsibilities include developing new clinical practicum experiences, revising existing curriculum, teaching, and serving on various committees. Again, as mentioned earlier, these are additional duties to their day-to-day responsibilities. In addition, clinical preceptors are held at a high standard because of the nature of our profession. Our profession is built on quality and accuracy. Therefore, clinical laboratory science preceptors have to be very competent in their own knowledge of the various clinical laboratory subjects to be able to teach students and to integrate their classroom experience with their clinical rotation.
“Clinical sites must value their preceptors and make every effort to obtain the resources needed to support their clinical laboratory scientists serving in that capacity.”
Professional Development
To be effective as a preceptor, and in the training of clinical laboratory students, it is imperative that preceptors remain current in their laboratory education. One way to remain current is to attend professional conferences. These conferences provide a wealth of educational resources to help develop and sharpen one’s teaching skills. Many individuals who serve as preceptors are motivated by a desire to teach and to prepare the next generation of clinical laboratory scientists. However, precepting students requires both time and resources, especially monetary resources to attend professional development opportunities such as ASCLS or ASCP conferences to improve on their teaching skills.
The current compensation model for preceptors does not include reimbursement for precepting and teaching, or for professional development. Clinical preceptors often rely on their own resources to travel to these various conferences. Clinical sites must value their preceptors and make every effort to obtain the resources needed to support their clinical laboratory scientists serving in that capacity.
The growth of the allied health professions has created challenges in education and training. One major concern is the number and quality of preceptors working with students in community health settings. The supply of preceptors has been shrinking, and this shortage has become a significant issue for health professions schools. Many have reported that preceptors are dropping out, and the schools cannot offer sufficient professional development, recognition, support, or financial rewards to entice them to stay (Beck Dallaghan et al., 2017; Rokusek, 2016).
The clinical laboratory science profession is dependent on these valuable professionals serving as preceptors who are committed and dedicated to training and educating CLS students. Many programs are finding ways and opportunities to identify resources of their own because they recognize the value of the preceptor. Some opportunities may include writing grants to help secure funding to send preceptors to professional development conferences. Also, being an advocate at the clinical placement site for additional incentives and resources that can help send these valuable individuals to conferences and workshops would mean a great deal to them and help retain them as preceptors for years to come.
Lloyd Josephat is program director for Clinical Laboratory Science and Clinical Pathologist Assistant Programs at the University of Alabama at Birmingham.
If you're interested in this topic, join the ASCLS Education Scientific Assembly.
