Volume 36 Number 6 | December 2022
Donna Showers, MS, MT(ASCP), FACHE, ASCLS Region V Government Affairs Committee Chair

The Institute of Medicine (IOM) has coined six aims for our healthcare system:
- Safe: Avoiding harm to patients from the care that is intended to help them.
- Effective: Providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and misuse, respectively).
- Patient-centered: Providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.
- Timely: Reducing waits and sometimes harmful delays for both those who receive and those who give care.
- Efficient: Avoiding waste, including waste of equipment, supplies, ideas, and energy.
- Equitable: Providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
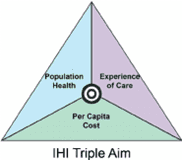
In their 2008 pivotal article for the Institute for Healthcare Improvement (IHI), Donald M. Berwick, Thomas W. Nolan, and John Whittington introduced a new term into the healthcare lexicon—the “Triple Aim.” This was a transformative new approach to improve population health. The Triple Aim has become foundational to valuebased care. According to the IHI, the goal of the Triple Aim is to:
- Improve the experience of the patient while under care
- Improve population health
- Lower per capita costs of healthcare.
As medical laboratory professionals, we should acknowledge and appreciate how the work that we do impacts these overarching healthcare aims. Just a few examples include:
- Safe: the right test for the right patient at the right time and quality assurance programs to reduce the risk of lab testing errors.
- Effective and Efficient: optimizing lab test utilization/stewardship—who knows this better than a medical laboratory professional?
- Patient-centered, Patient Experience, and Timely: medical laboratory professionals working to reduce testing turnaround time so results can improve the timeliness of clinical decisions.
- Equitable: there should be no bias—conscious or otherwise—in lab testing; blood is blood.
- Population Health: diabetes screening and monitoring, and sexual health lab testing impacts the physician’s ability to provide proactive healthcare and manage the health of the community.
- Lowering Per Capita Costs: clinical laboratory leaders are often engaged in LEAN transformation to reduce waste and take cost out of the system.
Value Based Purchasing (VBP)
If we define healthcare value as outcomes/cost, where outcomes include quality, efficacy, and safety and cost includes resources and dollars, you can quickly understand VBP.
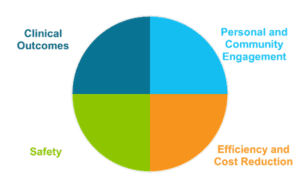
The Medicare Hospital VBP Program rewards or penalizes hospitals based on the quality of care provided in the inpatient hospital setting. Many private payers have also adjusted their reimbursement models to pattern after CMS’ VBP. The framework used to monitor and measure a hospital’s success with VBP includes quality metrics that fall into four categories, which continue to evolve over time:
- Clinical Outcomes: Measured by 30-day mortality rates for conditions such as certain cardiac diseases/procedures, pneumonia, COPD, and complications post hip/knee arthroplasty.
- Safety: Measured by rates of catheter-associated urinary tract infection (CAUTI), central line-associated blood stream infection (CLABSI), Clostridium difficile infection (CDI), Methicillin-resistant Staphylococcus aureus (MRSA), and surgical site infections.
- Personal and Community Engagement: Hospital Consumer Assessment of Healthcare Providers and Services (HCAHPS) scores
- Efficiency and Cost Reduction: Medicare spending/beneficiary
Performance in these areas can impact a hospital’s reimbursement for inpatient services by as much as 2 percent. The overarching principles of VBP are patient satisfaction, safety, outcomes, and cost. Laboratory services are crucial to success with VBP—our testing, algorithms, the speed and accuracy with which we deliver test results, and our constant evaluation and improvement of clinical laboratory operations in order to reduce waste and costs.
Also included in VBP is the Hospital Acquired Condition Reduction (HAC) program. This program penalizes the worst performing quartile of hospitals with a 1 percent reduction in reimbursement rates for patients who acquire the conditions listed in the Safety portion of VBP after three days of being admitted to a hospital. Again, laboratory professionals develop operations and algorithms (e.g., patient surveillance/screening for C. diff and MRSA/SA) that can aid hospitals in minimizing HACs.
Note: CMS is temporarily pausing most VBP penalties due to extraordinary circumstances caused by the COVID-19 pandemic. Some quality metrics data, however, is still being collected.
Patient Safety and Healthcare Provider Value: In Conclusion
If we take the time to think deeply about what is required to achieve the IOM healthcare aims, the IHI Triple Aim, and success in VBP programs, it becomes clear that the contribution from laboratory professionals is crucial to the mission. If we can broaden our thinking beyond accomplishing our day-to-day lab duties to include our contribution to the greater healthcare endeavor, we have a lot to feel proud about.
Clinical laboratory leaders should be in communication with their executive suites and have a seat at the table when quality metric scores are being reviewed. Our work has direct impact. And the next time you need to justify additional head count in your lab or the purchase of new capital equipment/testing programs, think about how you can approach your CFO with examples of how clinical laboratory scientists contribute to success with VBP and the Triple Aim. This should get their attention!
Donna Showers is a Clinical Value Executive for Cepheid in Sunnyvale, California.