Ian Wallace, MLS(ASCP)CM
Throughout our schooling, laboratory professionals are taught the importance of utilizing platelet and white blood cell (WBC) estimates to verify a potential analyzer error or an issue with the specimen tested. However, with how efficient analyzers have become, I have recognized that we repeatedly forget that estimates remain important—even if the analyzer is functioning correctly.
Take for instance, a 66-year-old male who came through the emergency department with a chief complaint of a headache. According to the patient’s wife, the male was consistently experiencing headache, fatigue, lethargy, decreased oral intake, dehydration, confusion, and felt “warm to the touch.” The patient stated he had a carcinoma removed a few weeks earlier and had symptoms “off and on” ever since. He visited an urgent care earlier in the week to discuss his symptoms, but nothing remarkable came back from his results. Patient admitted that he traveled a lot; he was not concerned that he encountered any insect bites, but he did have malaria when he was younger—from a visit to Africa. Now, you may think you know where this case is going, but I can assure you, you don’t.
Specimens received in the lab on this patient were a CBC, automated urinalysis, and a CMP. Of note, the patient had the following abnormal results:
| TEST | VALUE | REFERENCE RANGE |
|---|---|---|
| HCT | 39.4 | 40.0-54.0% |
| Platelet Count | 60 | 150-400 × 103/μL |
| Monocytes, Absolute | 1.18 × 103/μL | 0.00–1.00 × 103/μL |
| BUN | 21 | 7–18 mg/dL |
| Glucose, Serum | 122 | 70–100 mg/dL |
| Calcium | 8.4 mg/dL | 8.5–10.1 mg/dL |
| GFR Estimated | <60 | >60 |
| Albumin, Serum | 2.7 g/dL | 3.4–5.0 g/dL |
| Bilirubin, Direct | 0.3 | 0.0–0.2 mg/dL |
| Blood, Urine | Small | Negative |
While none of these values are critical, our hematology department has rules set in the middleware that are set to “flag” and reflex a slide review of any specimen that has a platelet count of <75 × 103/μL. The operator alert translates to, “Thrombocytopenia: Clot check. Scan slide and perform PLT estimate if first time on admission and add comment.”
This is where the story and the importance of estimates becomes very significant. When the specimen came off the analyzer, I checked the tube for a clot, and nope, no clot present. So, the specimen is acceptable. Next, I slid a slide under the scope.
I was taught when doing any type of review, always be on the lookout for abnormalities, even if you are simply scanning a slide. As I scan my slide, I am looking and can definitely agree that this patient is thrombocytopenic. However, just as I’m about to result out the patient, something catches the periphery of my eye.
As I start to look more, I know I need to call pathology immediately. Pathology asks if I can send them pictures of what I see. I send them the following:
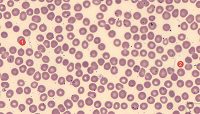 |
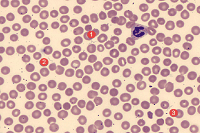 |
| Click here for a high-resolution image. | Click here for a high-resolution image. |
Pathology responded accordingly:
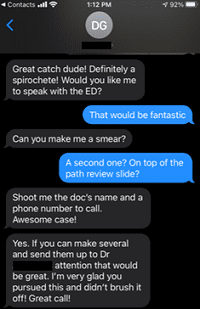 |
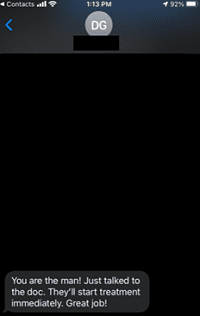 |
It was an incredible feeling to find Borrelia in a blood smear, especially as it had previously been missed since a slide review had never been performed. Even though we consulted infectious disease physicians, they never did decide to speciate the bug. However, the patient was placed on a 14-day dose of doxycycline and discharged the following morning.
Turns out, after some more investigation into the patient history, he lives on six acres in rural Colorado, which is most likely where they encountered the tick that bit him.
This case goes to show that even though we have become so accustomed to our top tier analyzers performing their jobs efficiently and effectively, they cannot identify everything. This further emphasizes the critical role we play as laboratory professionals in the healthcare setting.
Ian Wallace is a Medical Laboratory Scientist and Hematology Technical Specialist at Saint Joseph Hospital in Denver.
