Brandy Gunsolus, DCLS, MLS(ASCP)CM, ASCLS Patient Safety Committee Vice Chair, ASCLS Representative to the Coalition to Improve Diagnosis
 |
| The Coalition to Improve Diagnosis hosted an annual in-person meeting November 10-13 in Washington, D.C., where coalition representatives met to discuss what their organizations have been doing to improve diagnosis and to collaborate with other coalition members. |
 |
| Coalition representatives voted on eight potential priorities for the organization, with the top four priorities being the final focus. |
For those of you that may not be aware, this past year ASCLS joined the Coalition to Improve Diagnosis, a coalition of more than 80 societies, organizations, and facilities that have one common goal: to improve patient diagnosis. The ASCLS representative is chosen by the ASCLS Board of Directors from the active members of the Patient Safety Committee, and I am honored to have been chosen.
While the coalition does have several conference calls throughout the year, and has recently launched a MemberCentric community app very much like our own at ASCLS, it hosts an annual in-person meeting where coalition representatives are able to meet and discuss what their organizations have been doing to improve diagnosis, as well as develop opportunities to collaborate with other coalition members. This year’s coalition annual meeting was during the Diagnostic Error in Medicine Conference, November 10-13 in Washington, D.C. ASCLS was not the only new organization represented at the coalition meeting; there were 12 total new members, including COLA and The Joint Commission.
Each coalition representative provided a brief report of activities his or her organization has been working on toward improving patient diagnosis. Activities reported on behalf of ASCLS included:
- Develop patient safety brochures for both patients/caregivers and providers. These products are customizable for individual facilities to use and distribute to their own patients and providers to help both groups improve laboratory testing.
- Write patient safety articles for COLA’s Lab Testing Matters website.
- Volunteer for LabTestsOnline Consumer Response Team, answering questions of both patients and clinicians regarding laboratory testing.
- Oversee and support the Doctorate in Clinical Laboratory Science programs and practitioners.
- Develop podcasts and webinars, accessible to both laboratory and non-laboratory healthcare professionals, on a variety of topics, including topics related to improving patient safety.
Coalition Member Highlights
Interesting updates from other coalition members include (not a comprehensive list; only some pertinent highlights):
- American Health Quality Association – Currently working with Centers for Medicare & Medicaid Services (CMS) to identify and eliminate quality measures that have not produced quality healthcare improvements that were intended, as well as implement diagnostic quality measures.
- Centers for Disease Control and Prevention – Part of its project ECHO is a demo project to link laboratory professionals to clinicians through telemedicine to help eliminate the gap between physicians and the laboratory.
- ECRI Institute – Sent a survey to all National Provider Identifier (NPI) registered providers asking about various concerns in daily patient management; diagnostic error was the biggest concern identified in the survey. It has also established a database of genetic tests with evidence for what is clinically valid and clinically useful, which is currently used by both physicians and insurance payors.
- Geisinger – Developed a toolkit for clinical service directors to show them how to use diagnostic errors as learning tools in a non-threatening manner.
- MedStar – Implemented a review death within their health system by an interdisciplinary team to identify diagnostic errors and then identify where the diagnostic process can be improved to prevent such deaths in the future.
- Society to Improve Diagnosis in Medicine – Australia now has its own coalition with 50 members. Improving Diagnosis in Medicine Act of 2019, H.R.5014, was introduced in the House of Representatives by Representative Lujan and Representative Ray on November 8 before the coalition annual meeting. More information regarding this act will be forthcoming.
- Veterans Health Administration – Developing an algorithm to measure timeliness of test result follow-up by clinicians and plans to improve targets for improvement based on baseline measurements.
Grant Opportunity
The coalition is also tasked with developing guidance for Diagnosis Quality Improvement (DxQI) grants that will be awarded by the Gordon and Betty Moore Foundation, a coalition sponsor. These one-year renewable grants will be open to anyone who has an innovative and/or educational idea to improve diagnostic quality. Grants will be capped at $50,000 per proposal with a total of $3 million being awarded over the next three years.
At least 50 percent of awarded proposals must be directed towards improving diagnosis of cancer, infection, or acute vascular events. There was much talk about community, rural, and critical access perhaps having some preference for a percentage of grants as well. This will be an excellent opportunity for project funding for anyone who has a great idea. If you need help with grant writing, we have ASCLS members with grant writing knowledge who can help organize and edit any member wishing to submit.
Coalition Priorities
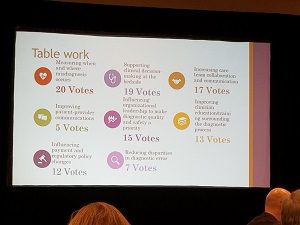
The last task for the coalition was to determine priority areas for coalition societies to focus on, and potentially partner together. There were eight potential priorities and each coalition representative was allowed to vote for three of these priorities, with the top four being the final focus. The themes that were up to a vote were:
- Measuring when and where misdiagnosis occurs
- Standardize event reporting and taxonomy
- Supporting clinical decision-making at the bedside
- Interdisciplinary workflows for diagnostic screening and follow-up
- Increasing care team collaboration and communication*
- Lead provider identified to decrease segmentation of care
- Influencing organization leadership to make diagnostic quality and safety a priority*
- To get to ROI/cost analysis on improving diagnostic quality
- Improving clinician education/training surrounding the diagnostic process*
- Influencing payment and regulatory policy changes
- Reducing disparities in diagnostic error
- Improving patient-provider communications
The bolded priorities were the priorities that won the vote with asterisked (*) priorities being the three priorities that I voted for as representative of ASCLS. Coalition members can, and should, continue to work on non-voted areas; however, the coalition’s big push for the next year will be on the top four voted priorities.
The coalition is looking for working group members from coalition organization members for each of these four priorities. These working group members do not have to be the organization’s coalition representative but should be someone who is very active at the top or national level of the organization. If anyone is interested in joining one of the coalition’s workgroups on the bolded priorities above, please contact me at brandy.gunsolus@gmail.com.
In summary, the work ASCLS has done toward improving patient safety and reducing diagnostic error has been great and well appreciated, but there is still much to do. We are just chipping at the top of the iceberg of diagnostic error. We have positioned ourselves by joining this amazing coalition to make a bigger impact than we ever could have imagined … it’s our responsibility to our profession and patients to do it.
Brandy Gunsolus is doctor of clinical laboratory science at Augusta University Medical Center in Augusta, Georgia.
